There have been a lot of discussions recently on clinical reasoning.
Clinical reasoning: The process by which practitioners collect and process information.
Clinical reasoning is a skill which can be learned, and taught. It’s an elusive concept, and involves both reasoning and pattern recognition, but it entails even more than that. It embodies experience and logic. For some, it comes easily, usually because reflective thinking has been taught from the beginning. For those who were taught in a more didactic environment, clinical reasoning may not come naturally, and needs to be consciously learned.
That’s all very well and good, but how do you actually teach clinical reasoning skills?
Here are some thoughts:
- Introduce the idea of Clinical Reasoning
- Gain insight into how clinicians come to a diagnosis
- Recognise key features and formulate illness scripts
- Use Compare and Contrast tables
- Promote Reflective practice
1. Introduce the idea of Clinical Reasoning
Discussing the concept is very useful. Essentially, clinical reasoning is the process of receiving information, sorting it into recognisable chunks and coming up with a list of possibilities and then testing those differentials. To this end, it is helpful to understand how our brains work when we are considering a clinical situation. That way we can deliberately enhance the process. Clinical reasoning is what we do all day every day, whether we’re aware of it or not.
2. Gain insight into how clinicians come to a diagnosis
It certainly is useful to be made aware of thought processes that occur when making a diagnosis. So let’s talk about how clinicians come to a diagnosis. There are generally 2 methods: either associative or analytical. Using the associative method, there is pattern recognition – a spot diagnosis. It’s instant, unconscious, based on experience and has a high risk of error. Using an analytical approach is deductive, slow and deliberate, based on books and research and has lower risk of error. Good clinicians use both methods!
It’s also useful to address the whole concept of cognitive biases, and this can be done by using examples and role plays. There are so many cognitive biases or errors that can come into play, and being aware of potential biases means that they are more likely to be recognised and addressed. Cognitive biases include availability (relying on the diagnosis that easily comes to mind), framing (being influenced by how the information is presented), blind obedience (believing that what was said by the expert is correct), anchoring (fixing on your original idea), confirmation (paying attention only to the findings that support your diagnosis) and premature closure (prematurely stopping the diagnostic process when you think you have the correct answer).
3. Recognise key features and formulate “illness scripts”
Taking a comprehensive history is a fundamental skill for a general practitioner. Identifying the key features helps get to the crux of the matter, and is a skill that’s tested in the RACGP KFP and OSCE exams, and ACRRM’s StAMPs, and is therefore useful to know! Identifying key features will help differentiate one diagnosis from another. A good way to teach this is to prepare typical patient narratives and ask registrars to identify the key features. You can then change the scenario slightly by changing the age, the gender, the ethnicity or the timeframe and re-consider the problem. This demonstrates how important it is to take note of these key features.
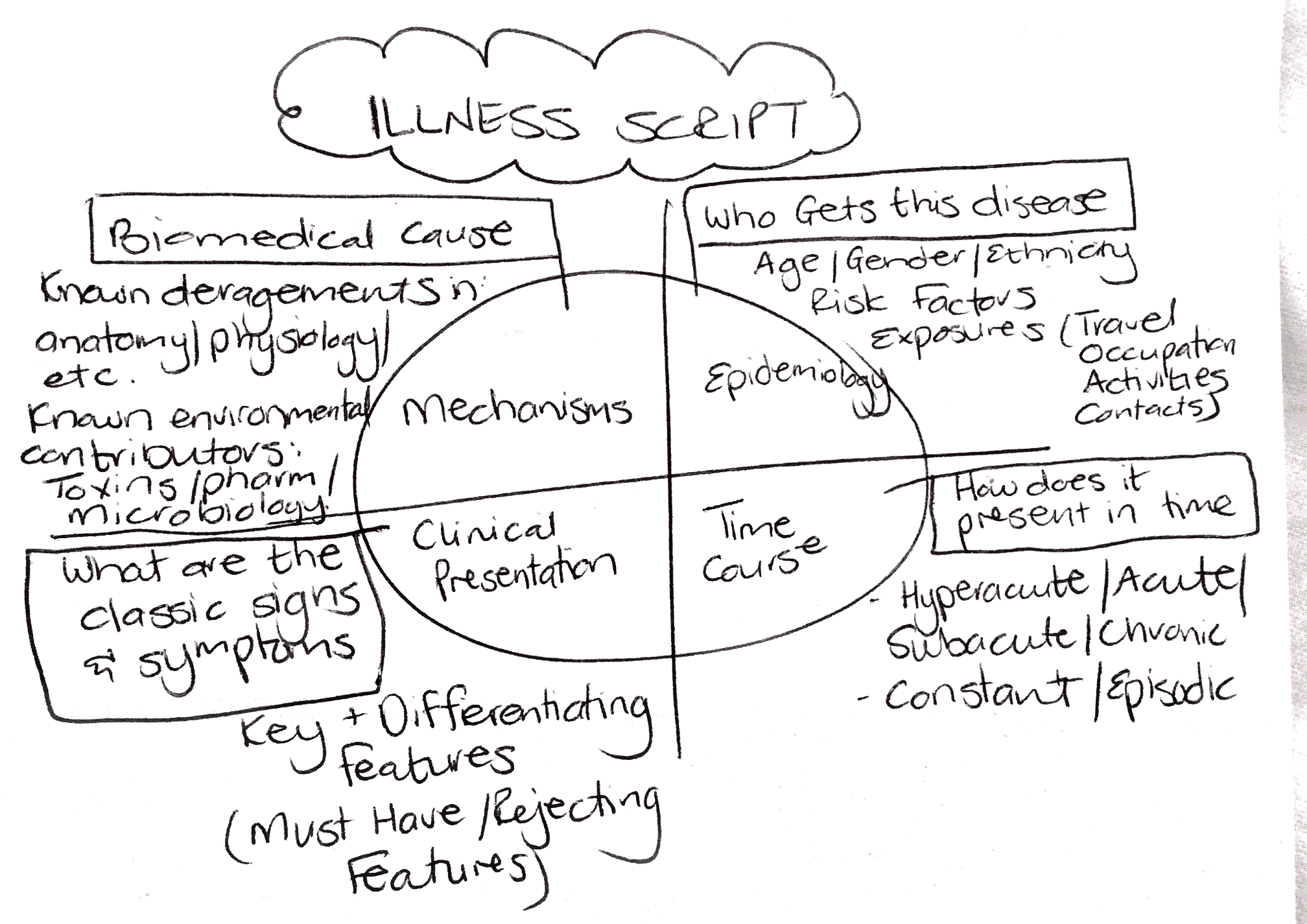
Learning to translate what patients say to illness scripts makes the story more like a text book presentation and aids in producing a differential diagnosis. Patients don’t speak in illness scripts, so we need to translate what they say into medical terms that will stimulate our memory. Collecting data for an illness script can be summarized as such:
4. Use Compare and Contrast tables
Compare and contrast tables assist in clinical decision making by reinforcing connections between new and previously stored information. Practically, this can be done by discussing a clinical case and producing a differential diagnosis list, and then using the table to compare 3 of the differentials by highlighting only the important points in each differential. It will then make it easier to prioritise differentials into most likely, uncertain and unlikely diagnoses. Here’s an example.
5. Promote Reflective practice
At a recent RVTS workshop, we had a great session on clinical reasoning where registrars were given different clinical scenarios and asked to identify key features, write an illness script and recognise cognitive biases. This made for great conversations and learning, and further discussion around the following questions led to greater insights.
- “Can you remember a diagnostic situation where you realised you didn’t know something, and needed to know it?”
- Can you describe what happened?
- What prompted you to recognise this?
- How do you know you are making the right diagnosis in a consultation?
Teaching clinical reasoning is exciting and challenging. Using these 5 steps outlined, it is possible to teach this essential skill. We’d be interested in hearing any other tips and techniques you’ve come across to teach clinical reasoning.
References:
I came across some really good resources while looking into this topic:
This great AFP article on Clinical Reasoning
UTAS has a “Clinical Reasoning Instructor Resource” with some practical tips



Leave a Reply